The Mismanagement of ASCVD: Richard Z. Cheng, M.D., Ph.D., Thomas E. Levy, M.D., J.D.
Abstract
We have documented the reversal of 10 cases of cardiovascular diseases, including two with up to 70% coronary artery stenosis, through an integrative orthomolecular medicine approach addressing root causes(1). This evidence supports the view that atherosclerotic cardiovascular disease (ASCVD) is fundamentally an inflammatory condition beginning at the endothelium. In contrast, the prevailing cholesterol-lowering paradigm overly simplifies ASCVD management, focusing on intermediary markers while neglecting foundational drivers such as diet, inflammation, environmental toxins, and nutrient deficiencies. Root Cause Analysis (RCA), a proven methodology for addressing complex problems, remains underutilized in ASCVD care. This paper critiques the reliance on symptom management and highlights the barriers in the drug-based medical symptom-relief system, including corporate influences, that perpetuate preventable suffering. We call for the integration of RCA and holistic strategies to address ASCVD’s underlying causes and restore public trust in healthcare institutions.
Introduction
Modern problem-solving methodologies emphasize addressing the root causes rather than merely managing symptoms(2). Root Cause Analysis (RCA) is a cornerstone of this approach, offering structured methods to identify the origins of complex problems and implement long-term solutions. Despite its proven effectiveness, RCA is glaringly absent in ASCVD management. Instead, institutions like the American Heart Association (AHA) champion symptom-focused interventions, notably statins, fostering dependency and yielding suboptimal outcomes(3,4). This paper critiques this neglect of RCA in ASCVD care, questioning whether it results from ignorance, incompetence, or deliberate profit-driven collusion with pharmaceutical interests.
RCA involves defining the issue, gathering relevant data, analyzing causes using tools like the “Five Whys,” and implementing targeted solutions while monitoring results(5–7). When applied to ASCVD, RCA highlights neglected systemic issues such as poor diet, chronic inflammation, environmental toxins, and nutritional deficiency, which are often sidelined in favor of pharmaceutical approaches.
AHA’s Oversimplified Approach to ASCVD Risk Factors
AHA fails to adequately categorize ASCVD risk factors into root causes, intermediary steps (mechanisms), and clinical outcomes. Instead, it lumps these factors together into broad categories without acknowledging their distinct roles in disease development and progression(8). This lack of differentiation reflects a fundamental ignorance of the Root Cause Analysis (RCA) process, or worse, an intentional effort to obscure root causes to maintain the status quo.
Root causes—such as poor diet, chronic inflammation, environmental toxins, and nutritional deficiencies—are foundational contributors that drive the mechanisms leading to ASCVD. Intermediary steps include processes like endothelial dysfunction, oxidative stress, lipid dysregulation, and deposition, which translate these root causes into measurable clinical markers. Clinical outcomes, such as myocardial infarction, stroke, and peripheral artery disease, represent the end stage of these pathological processes.
By failing to make these distinctions, the AHA perpetuates a misguided focus on intermediary markers like LDL cholesterol while ignoring upstream drivers of disease. This oversimplification undermines efforts to address ASCVD at its source and instead promotes symptom management, often through pharmaceutical interventions like statins. This approach, at its best, reveals a lack of understanding of complex disease processes. At its worst, it suggests an intentional burying of root causes, bordering on criminal negligence by prioritizing profit over patient health.
The AHA’s Symptom-Focused Paradigm
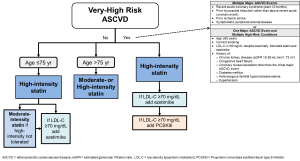
The AHA and its endorsed guidelines exemplify a symptom-focused approach to ASCVD management, prioritizing LDL cholesterol reduction through statins while neglecting the root causes of the disease(9). This strategy oversimplifies the complexity of cardiovascular disease and does not adequately address foundational contributors such as poor diet, chronic inflammation, environmental toxins and nutritional deficiencies. While statins have demonstrated efficacy in reducing certain cardiovascular events, a singular focus on LDL cholesterol fails to incorporate a more holistic understanding of ASCVD pathophysiology. This lack of emphasis on root causes highlights a significant gap in current guidelines and underscores the need for integrating Root Cause Analysis (RCA) to develop more comprehensive, patient-centered approaches to ASCVD care.
- Dietary Misdirection: The AHA’s long-standing endorsement of low-fat (and consequently high-carbohydrate) diets may have inadvertently contributed to the obesity and diabetes epidemics, which are significant drivers of ASCVD(10–15). Emerging evidence indicates that low-carb, anti-inflammatory diets can effectively reverse metabolic syndrome and improve cardiovascular health(16–19). Contrary to the AHA’s long-term advocacy of low-fat diets, studies increasingly show that high-fat ketogenic diets support weight loss, enhance glycemic control, improve lipid profiles and insulin resistance, and reduce inflammation(20–23). Ketogenic diet has been suggested to improve cardiac energetics, reduce oxygen use(24) and even reverse atherogenic dyslipidemia(25). The continued promotion of outdated dietary guidelines reflects a reluctance to adapt to evolving nutritional science, highlighting a critical gap in ASCVD prevention efforts.
- Neglect of Inflammation: Chronic inflammation is a well-documented root cause of ASCVD, yet the AHA focuses narrowly on LDL cholesterol(26–28). Chronic oral pathogen colonization in the coronary artery wall has been consistently present, accounting for the chronic inflammation always seen in coronary artery diseas(29–39). This omission raises questions about the integrity of guidelines shaped by pharmaceutical interests.
- Suppression of Environmental Factors: Toxins are pervasive in modern life, from industrial chemicals to pollutants, and many have cardiotoxic effects. They damage mitochondria, increase oxidative stress, and disrupt cellular energy production, contributing to cardiovascular diseases through processes like endothelial dysfunction and lipid peroxidation. Heavy metals and certain drugs exemplify how toxins exacerbate oxidative stress and mitochondrial damage, emphasizing the need to address their impact on heart health(40–43). The AHA’s silence on these contributors suggests either ignorance or a refusal to address non-pharmaceutical solutions.
- Overlooking Nutritional Deficiencies: Deficiencies in essential nutrients, such as vitamin C and magnesium, are critical yet often overlooked contributors to ASCVD. By neglecting these and other nutrient deficiencies, the AHA’s approach fails to address key modifiable factors in disease progression. While many vitamins and micronutrients play important roles in heart health and ASCVD management, the following examples illustrate their significance:
- Vitamin C: Linus Pauling’s unified theory highlights the centrality of vitamin C in maintaining vascular integrity(44,45). He proposed that chronic vitamin C deficiency underpins atherosclerosis by impairing collagen synthesis, which is vital for the structural integrity of arterial walls. This deficiency weakens arteries, making them prone to damage and plaque formation.
- Magnesium: This critical mineral supports endothelial function, regulates blood pressure, and prevents arterial calcification. Magnesium deficiency is associated with increased cardiovascular risk but remains inadequately addressed in mainstream guidelines(46).
- The Role of Big Pharma in ASCVD Mismanagement: The influence of pharmaceutical companies on ASCVD management is significant and raises important concerns. Statins, generating billions in annual revenue, illustrate how financial incentives can shape treatment priorities, emphasizing symptom management over root cause resolution.
- Financial Conflicts of Interest: Studies reveal that 56-90% of guideline authors have financial relationships with drug companies(47–49). A systematic review found over half of guideline authors had industry ties, particularly in areas where pharmaceuticals dominate treatment(50,51). Many guideline panels lack formal processes for declaring conflicts of interest, with only 2 out of 44 reviewed guidelines containing specific disclosures(47). Undisclosed financial relationships were identified in 24% of authors who claimed no conflicts and 70% of guidelines(52).
- Impact on Care: Industry ties may influence guideline recommendations, potentially leading to overdiagnosis and overtreatment(53,54). Additionally, organizations producing guidelines often maintain financial relationships with the pharmaceutical industry, further complicating impartiality(55).
- Specific Concerns in ASCVD Guidelines: Many researchers and institutions that shape ASCVD guidelines receive funding from statin manufacturers(56–60). Industry tactics to influence guidelines include funding biased research, lobbying, and employing sophisticated marketing strategies targeting both physicians and the public(56,58). These practices create significant conflicts of interest, undermining public trust in the objectivity and credibility of clinical guidelines.
- Suppression of Alternatives: Non-pharmaceutical interventions, such as dietary changes, are often marginalized in favor of pharmaceutical treatments, despite substantial evidence supporting their efficacy(61–63). For example, recent research has demonstrated the benefits of low-carb, high-fat diets in improving metabolic health, challenging traditional low-fat dietary recommendations(10–15). However, these approaches remain underutilized in mainstream healthcare, reflecting a systemic bias toward pharmaceutical solutions. The lack of emphasis on Root Cause Analysis (RCA)-driven strategies represents a critical gap in addressing underlying contributors to ASCVD. Expanding the integration of non-pharmaceutical interventions, including dietary changes, exercise, and stress management, requires a shift in focus toward holistic, patient-centered care and increased funding for lifestyle-focused research. Addressing this oversight is essential for improving long-term health outcomes and reducing reliance on medication.
- Public Misrepresentation: By emphasizing statins as the primary solution, the AHA’s guidelines risk overshadowing the critical roles of systemic factors such as diet and environmental toxins in ASCVD development. While statins have demonstrated benefits in reducing cardiovascular events, focusing exclusively on pharmaceutical interventions neglects the broader context of disease prevention and management. Addressing these systemic issues alongside medication could lead to more comprehensive and sustainable health outcomes.
The Case for RCA in ASCVD Management
Adopting RCA in ASCVD care is not only logical but also essential for addressing the root causes of disease and improving patient outcomes. Our integrative orthomolecular medicine approach exemplifies this comprehensive care model(64). Ignoring this approach leads to missed opportunities for effective prevention and care. The key benefits of RCA include:
- Addressing Root Causes: Poor diet, chronic inflammation, environmental toxins, and deficiencies of vitamins and micronutrients can be effectively identified and mitigated through RCA-driven strategies. For example, addressing vitamin C and magnesium deficiencies has been shown to improve vascular health and reduce ASCVD risk.
- Reducing Dependency on Drugs: By prioritizing prevention and lifestyle changes, RCA minimizes the need for lifelong medications, which are often associated with significant side effects. For instance, low-carb diets and anti-inflammatory interventions can reduce reliance on statins and other pharmaceuticals.
- Enhancing Public Trust: Transparent, RCA-based guidelines that prioritize holistic care would restore faith in healthcare institutions, demonstrating a commitment to addressing the systemic causes of ASCVD rather than focusing solely on symptom management.
Case Study: RCA vs. Symptom Management in ASCVD
Traditional approaches to ASCVD management often involve prescribing statins to lower LDL cholesterol, focusing on symptom control rather than addressing underlying causes. In contrast, an RCA-based approach seeks to identify and mitigate root causes of the disease through(64):
- Investigating Root Causes: Assess dietary habits through food logs and nutrient panels, evaluate environmental exposures (e.g., heavy metals or pollutants), and identify deficiencies in key micronutrients such as vitamin C and magnesium.
- Implementing Lifestyle Changes: Introduce low-carb, raw or minimally processed, adequate healthy fat, anti-inflammatory diets to enhance metabolic health and implement toxin reduction strategies tailored to the patient’s exposure history.
- Supplementing with Key Nutrients: Provide evidence-based supplementation, including vitamin C for vascular health, magnesium for endothelial function, and omega-3 fatty acids to reduce inflammation.
- Monitoring Systemic Markers: Use inflammatory markers such as C-reactive protein (CRP) to track progress and adjust interventions as needed.
This approach not only addresses root causes but also empowers patients to take control of their health, reducing dependence on pharmaceutical interventions.
A more detailed analysis of each of these areas will be discussed in future papers.
Conclusion:
The failure to incorporate Root Cause Analysis (RCA) into ASCVD management represents a significant oversight in modern medicine’s priorities. While the AHA’s symptom-focused guidelines can be effective in managing certain aspects of ASCVD, they often neglect the underlying drivers of the disease, perpetuating dependency on pharmaceuticals and preventable suffering.
Integrating RCA into healthcare would enable a more comprehensive approach, addressing root causes such as poor diet, chronic inflammation, environmental toxins, and nutritional deficiencies. This shift has the potential to improve patient outcomes, reduce reliance on medications, and, in some cases, prevent or even reverse ASCVD, as demonstrated in our case reports.
Challenges to adopting RCA, including resource constraints, clinician education, and systemic inertia, are significant but surmountable through collaborative efforts. Overcoming these barriers will require interdisciplinary partnerships, updated clinical guidelines, and a commitment to patient-centered care. It is time for healthcare systems to embrace RCA as a cornerstone of effective, ethical, and holistic ASCVD management.
References: The Mismanagement of ASCVD: A Call for Root Cause Solutions Beyond Cholesterol







